Factors Influencing Severity and Impact of Symptoms in Patients with Upper Respiratory Tract Infection at Community Hospitals and Health-Promoting Hospitals
DOI:
https://doi.org/10.33192/Smj.2021.66Keywords:
Upper respiratory tract infection, health literacy, nutritional status, sleep quality, severity and impact of symptomsAbstract
Objective: This study aimed to examine the factors that influence the severity and impact of symptoms in patients with an Upper Respiratory Tract Infection (URTI).
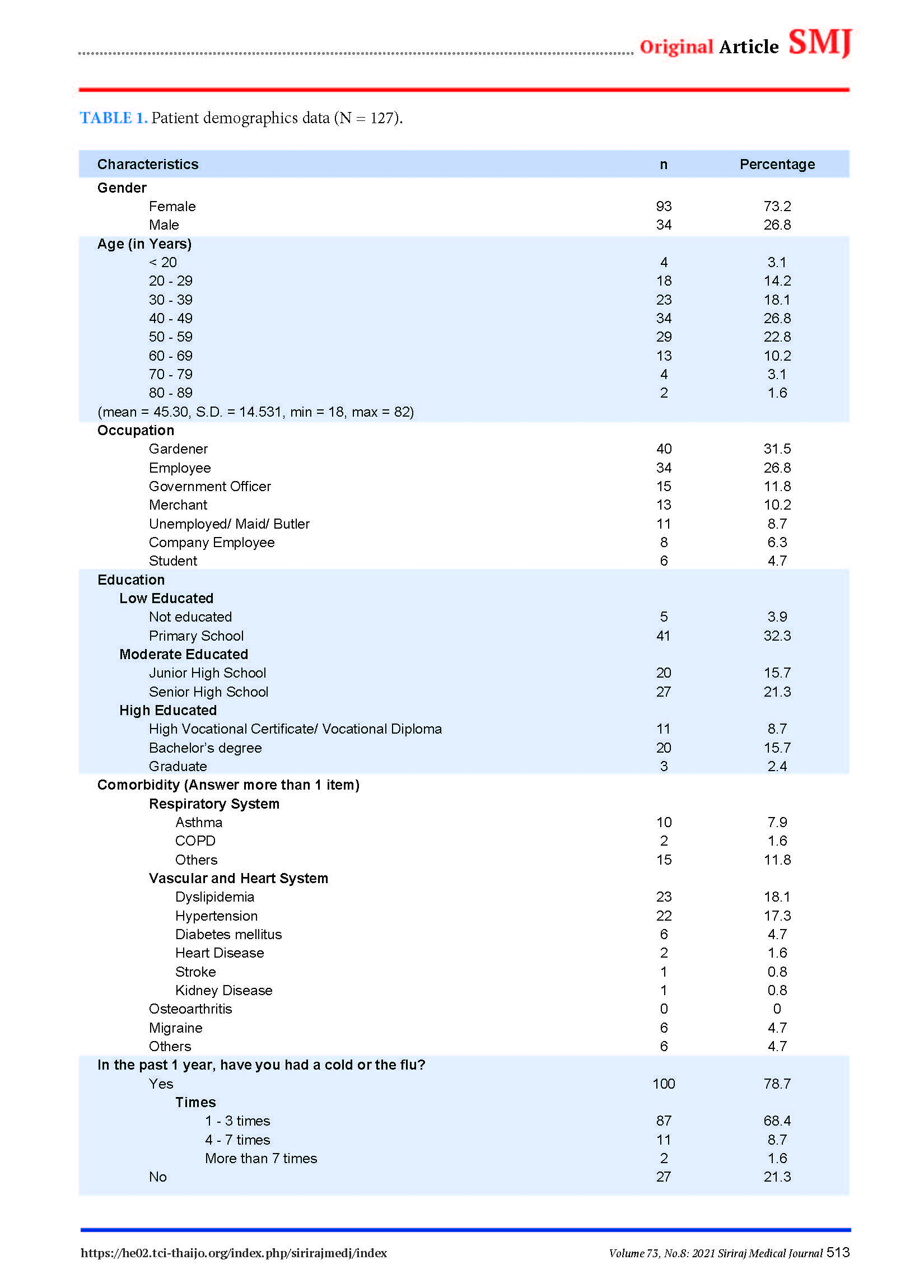
Materials and Methods: This study is a correlational predictive research. The sample size included 127 patients with URTI accessing care at community hospital and 5 health-promoting hospitals from February to June in 2020. Data were collected by using a questionnaire on demographic data, a questionnaire on health literacy, a questionnaire on self-care behavior in patients with URTI, the Nutrition Alert Form (NAF), the Pittsburgh Sleep Quality Index (PSQI), and the Wisconsin Upper Respiratory Symptom Survey-21 (WURSS-21). Subsequently, the data were analyzed using descriptive statistics and multiple regression analysis.
Results: The sample had a mean age of 45.30 years in which 73.2% were females; the average score of severity and impact of symptoms was minimal (Mean = 52.75 ± 22.85). The results from the multiple regression analysis indicated that all variables were able to co-predict the severity and impact of symptoms in patients with URTI as 25.9% (R2 = .259, F = 10.676, p < .05). Sleep quality and health literacy were the most statistically significant in predicting the severity and impact of symptoms in this sample group (β = .393 and -.221 respectively, p < .05).
Conclusion: The findings suggested that nurses should encourage their patients to be aware of the importance of sleep, promoting a good sleep method and health literacy in order to make better decisions in their daily health.
References
Thomas M, Koutsothanasis GA, Bomar PA. Upper respiratory tract infection. Treasure Island: Stat Pearls Publishing LLC; 2020.
Turner RB. The common cold. 8th ed. Canada: Elsevier Saunders; 2015.p.748-52.e2
Rajaram S, Wiecek W, Lawson R, Blak B, Zhao Y, Hackett J, et al. A retrospective observational analysis of post-pandemic influenza-related outcomes in the United Kingdom, 2010-2014. Hum Vaccin Immunother 2018;14:368-77.
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789-858.
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88.
Duda K. Groups at high risk for dangerous flu complications: Verywell Health; 2020 [cited 2020 Aug 5]. Available from: https://www.verywellhealth.com/people-at-high-risk-for-flu-complications-770497.
Clement S, Ibrahim S, Crichton N, Wolf M, Rowlands G. Complex interventions to improve the health of people with limited literacy: A systematic review. Patient Educ Couns 2009;75:340-51.
Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ 2010;29:1-28.
British Columbia Health. Self care during an influenza pandemic. Pandemic Influenza Series 2006;250:62-69.
Morais AHdA, Aquino JdS, Silva-Maia JKd, Vale SHdL, Maciel BLL, Passos TS. Nutritional status, diet and viral respiratory infections: Perspectives for SARS-CoV-2. Br J Nutr 2020:1-12.
Besedovsky L, Lange T, Born J. Sleep and immune function. Pflugers Arch 2012;463:121-37.
Cohen S, Doyle WJ, Alper CM, Janicki-Deverts D, Turner RB. Sleep habits and susceptibility to the common cold. Arch Intern Med 2009;169:62-67.
Trongsakul S, Lambert R, Clark A, Wongpakaran N, Cross J. Development of the Thai version of Mini-Cog, a brief cognitive screening test. Geriatr Gerontol Int 2015;15:594-600.
Health Education Division. Health literacy and health behavior among of volunteers and working-age people; 2018 [cited 2019 July 18]. Available from: http://www.hed.go.th/linkHed/372
Shangyom D, Detprapon M, Malathum P. Self-care behaviors in older persons with upper respiratory tract infection. Rama Nurs J 2019;24:345-60.
Komindr S, Tangsermwong T, Janepanish P. Simplified malnutrition tool for Thai patients. Asia Pac J Clin Nutr 2013;22:516-21.
Sitasuwan T, Bussaratid S, Ruttanaumpawan P, Chotinaiwattarakul W. Reliability and validity of the Thai version of the Pittsburgh Sleep Quality Index. J Med Assoc Thai 2014;97:S57-S67.
Barrett, B. Wisconsin Upper Respiratory Symptom Survey - 21 - Daily Symptom Report; 2004 [cited 2019 July 15]. Available from: https://www.fammed.wisc.edu/files/webfm-uploads/ documents/research/wurss-21.pdf
Malathum P, Palaban S, Hanucharurnkul S, Achananuparp S. Symptom experiences and management strategies in adults with common cold or influenza. Rama Nurs J 2548;11:84-99.
Denlinger LC, King TS, Cardet JC, Craig T, Holguin F, Jackson DJ, et al. Vitamin D supplementation and the risk of colds in patients with asthma. Am J Respir Crit Care Med 2016;193:634-41.
Ibrahim HK, Elkady HM. Self-care practices of common cold and influenza among the elderly in alexandria, egypt. IJSR 2016;5:881-7.
Thielmann A, Gerasimovska-Kitanovska B, Buczkowski K, Koskela TH, Mevsim V, Czachowski S, et al. Self-care for common colds by primary care patients: A European multicenter survey on the prevalence and patterns of practices-The COCO study. Ecam 2016:1-9.
Goldberg DS, McGee SJ. Pain as a global public health priority. BMC Public Health 2011;11:770-4.
Kutner M, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education Statistics; 2006.
Sun X, Shi Y, Zeng Q, Wang Y, Du W, Wei N, et al. Determinants of health literacy and health behavior regarding infectious respiratory diseases: A pathway model. BMC Public Health 2013;13:1-8.
Bennett IM, Chen J, Soroui JS, White S. The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults. Ann Fam Med 2009;7:204-11.
Omachi TA, Sarkar U, Yelin EH, Blanc PD, Katz PP. Lower health literacy is associated with poorer health status and outcomes in chronic obstructive pulmonary disease. J Gen Intern Med 2013;28:74-81.
Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally assessed sleep and susceptibility to the common cold. Sleep 2015;38:1353-9.
Tongo M, Sy R. The Relation of Nutritional Assessment and Pneumonia Severity Index among Elderly Patients with Community Acquired Pneumonia Admitted at Cardinal Santos Medical Center. J Nutr Diet Suppl 2017;1:1-7.
Gatlin PK, Insel KC. Severity of type 2 diabetes, cognitive function, and self-care. Biological Research for Nursing 2015;17:540-8.
Downloads
Published
How to Cite
Issue
Section
License
Users are free to share, copy, and redistribute all articles published in the Siriraj Medical Journal (SMJ) in any medium or format as long as you follow the following terms:
- Attribution — You must give appropriate credit, provide a link to the material, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the publisher endorses you or your use.
- NonCommercial — You may not use the material for commercial purposes.
- NoDerivatives — If you remix, transform, or build upon the material, you may not distribute the modified material.
- No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.










